The Affordable Care Act’s Effects on Health Insurance Coverage
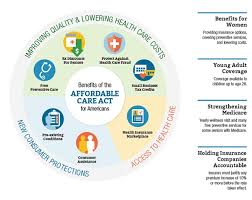
The main objectives of the Affordable Care Act (ACA), which was signed into law in 2010 under President Barack Obama, were to increase access to health insurance and raise the standard of care. Its provisions significantly altered the U.S. health insurance market and had far-reaching effects on both individuals and insurers.
The influence of the Affordable Care Act (ACA) on health insurance coverage is examined in this article, along with how it changed the dynamics of healthcare markets, increased insurance accessibility, and enhanced affordability.
Extension of Coverage for Health Insurance
Increasing the number of Americans with health insurance was one of the main objectives of the Affordable Care Act. More than 40 million Americans lacked health insurance prior to the Affordable Care Act, and millions more had coverage that was either insufficient or prohibitively expensive. In order to close this gap, the law established a number of crucial procedures.
Medicaid Expansion: Under the Affordable Care Act, states could choose to extend Medicaid to all people earning up to 138% of the federal poverty threshold. The federal government provided states with more funds to encourage them to expand Medicaid, despite the Supreme Court’s initial ruling that states could not be forced to do so.
By 2024, 39 states and the District of Columbia have embraced Medicaid expansion. Millions of low-income people were covered by this expansion.
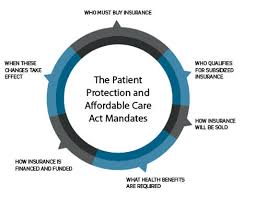
Health Insurance Marketplaces: The Affordable Care Act (ACA) created Health Insurance Marketplaces, or Exchanges, where people and small companies could shop for insurance if they were ineligible for Medicaid or employer-sponsored coverage.
The purpose of these marketplaces is to simplify and increase transparency in the process of buying health insurance. In order to make health coverage more affordable for those who previously couldn’t afford it, the Affordable Care Act (ACA) also established subsidies to assist lower-income individuals and families in paying premiums and out-of-pocket expenses.
Individual Mandate: The Affordable Care Act (ACA) imposed an individual mandate that compelled the majority of Americans to purchase health insurance or pay a penalty in order to promote participation in the health insurance marketplaces.
Under President Trump’s administration, the penalty was lowered to $0 in 2019, however initially the mandate helped increase the risk pool by bringing Insurance Market Reforms.
The Affordable Care Act (ACA) implemented a number of changes that increased the availability of health insurance for disadvantaged groups, such as people with preexisting medical problems. Prior to the Affordable Care Act, those with long-term conditions or past health problems sometimes faced expensive premiums or were denied coverage.
The statute forbade insurers from raising premiums based on health status and from refusing coverage due to preexisting conditions. As a result, more people, even those with medical issues, were able to obtain and maintain coverage.
Effect on Rates of Coverage
The number of Americans without health insurance has dramatically dropped since the ACA’s implementation. As a result of Medicaid expansion, the U.S. Census Bureau reports that the number of Americans without health insurance decreased from 16% in 2010 to about 8% in 2019.
Affordable Care
About 31 million Americans were enrolled in ACA-compliant health insurance plans, such as those offered by Medicaid, the marketplaces, and employer-sponsored insurance plans that complied with ACA standards, according to a 2023 Kaiser Family Foundation (KFF) study.
With the uninsured rates for Black and Latino populations falling more precipitously than those for White Americans, the Affordable Care Act has also been credited with reducing racial and ethnic gaps in health coverage.
Affordability has improved.
The Affordable Care Act (ACA) sought to increase access to insurance while also making it more affordable. Many Americans struggled to keep continuous coverage due to unaffordable premiums and out-of-pocket expenses prior to the Affordable Care Act. A number of initiatives were implemented by the bill to lower the cost of healthcare:
Marketplace Plan Subsidies: Under the Affordable Care Act, individuals who buy insurance through the Health Insurance Marketplaces are eligible for income-based subsidies, often known as premium tax credits. Americans with low and intermediate incomes have been able to afford coverage thanks in large part to these subsidies.
For instance, subsidies that lower monthly premiums are available to people who make between 100% and 400% of the federal poverty level (FPL). The American Rescue Plan Act (ARPA) temporarily raised these subsidies in 2021 and 2022, further lowering the cost of coverage during the COVID-19 epidemic.
Cost-Sharing Reductions (CSRs): The Affordable Care Act (ACA) provides low-income people with cost-sharing reductions, which lower out-of-pocket expenses for medical treatments such copayments, deductibles, and coinsurance, in addition to premium subsidies. This clause guarantees that people with low salaries won’t encounter financial obstacles.
Elimination of Lifetime and Annual Coverage Limits: Prior to the Affordable Care Act, many insurance policies had lifetime and annual coverage limits, which meant that the insurer would cease to pay if a policyholder’s medical costs reached a predetermined amount. By outlawing these caps, the Affordable Care Act made sure that those with costly or long-term medical issues would not lose their coverage if they reached them.
The ACA’s Drawbacks and Rebuttals
The ACA has encountered difficulties and criticism in spite of its achievements. Among the most important concerns are:
Increasing Deductibles and rates: Despite the Affordable Care Act’s goal of lowering health insurance costs, many Americans still have to pay exorbitant rates, especially for plans bought via the Health Insurance Marketplaces. Premiums went up in certain areas, particularly for middle-class families that did not State-Level Opposition to Medicaid Expansion.
Millions of low-income people lack access to reasonably priced healthcare since a sizable portion of states decided against expanding Medicaid. Because it has left a coverage gap for those who make too much to be eligible for Medicaid in states that have not expanded but not enough to purchase marketplace insurance, this move has generated controversy.
The repeal of the individual mandate penalty in 2019 raised worries that the risk pool for the Affordable Care Act would become less balanced as more sick people join the market and fewer healthy people enroll. Premiums for those who stay in the market may increase as a result.
In conclusion
The United States’ health insurance coverage has been significantly impacted by the Affordable Care Act.
Policymakers are still debating how to strengthen and expand the Affordable Care Act (ACA). Some are calling for changes like Medicare for All or the creation of a public option to further lower costs and increase coverage.
Although there will probably be ongoing discussions over the future of healthcare in America, there is no denying that the Affordable Care Act has had a significant impact on the current state of health insurance coverage.
